what refers to erratic, irregular contractions of the cardiac muscle
| Arrhythmia | |
|---|---|
| Other names | Cardiac arrhythmia, cardiac dysrhythmia, irregular heartbeat, heart arrhythmia |
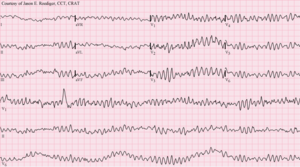 | |
| Ventricular fibrillation (VF) showing disorganized electrical activeness producing a spiked tracing on an electrocardiogram (ECG) | |
| Specialty | Cardiology |
| Symptoms | Palpitations, lightheadedness, passing out, shortness of breath, chest pain[ane] |
| Complications | Stroke, heart failure[two] [three] |
| Usual onset | Older age[4] |
| Types | Actress beats, supraventricular tachycardias, ventricular arrhythmias, bradyarrhythmias[3] |
| Causes | Problems with the electric conduction organisation of the heart[2] |
| Diagnostic method | Electrocardiogram, Holter monitor[5] |
| Treatment | Medications, medical procedures (pacemaker), surgery[6] |
| Frequency | Millions[4] |
Arrhythmias, also known every bit cardiac arrhythmias, heart arrhythmias, or dysrhythmias, are irregularities in the heartbeat, including when it is too fast or too slow.[2] A middle rate that is too fast – in a higher place 100 beats per infinitesimal in adults – is called tachycardia, and a heart rate that is too slow – below 60 beats per infinitesimal – is called bradycardia.[2] Some types of arrhythmias have no symptoms.[1] Symptoms, when nowadays, may include palpitations or feeling a suspension between heartbeats.[1] In more serious cases, there may be lightheadedness, passing out, shortness of jiff or breast pain.[i] While about cases of arrhythmia are not serious, some predispose a person to complications such as stroke or centre failure.[2] [3] Others may result in sudden decease.[iii]
Arrhythmias are ofttimes categorized into four groups: actress beats, supraventricular tachycardias, ventricular arrhythmias and bradyarrhythmias.[3] Extra beats include premature atrial contractions, premature ventricular contractions and premature junctional contractions.[3] Supraventricular tachycardias include atrial fibrillation, atrial flutter and paroxysmal supraventricular tachycardia.[3] Ventricular arrhythmias include ventricular fibrillation and ventricular tachycardia.[iii] [7] Bradyarrhythmias are due to sinus node dysfunction or atrioventricular conduction disturbances.[8] Arrhythmias are due to problems with the electrical conduction organisation of the heart.[two] A number of tests tin can help with diagnosis, including an electrocardiogram (ECG) and Holter monitor.[5]
Many arrhythmias can be effectively treated.[2] Treatments may include medications, medical procedures such every bit inserting a pacemaker, and surgery.[half dozen] Medications for a fast center rate may include beta blockers, or antiarrhythmic agents such as procainamide, which try to restore a normal eye rhythm.[6] This latter group may have more significant side effects, especially if taken for a long menstruation of fourth dimension.[six] Pacemakers are ofttimes used for slow heart rates.[half dozen] Those with an irregular heartbeat are oft treated with blood thinners to reduce the risk of complications.[6] Those who have severe symptoms from an arrhythmia or are medically unstable may receive urgent treatment with a controlled electrical shock in the course of cardioversion or defibrillation.[6]
Arrhythmia affects millions of people.[4] In Europe and North America, as of 2014, atrial fibrillation affects near 2% to 3% of the population.[9] Atrial fibrillation and atrial flutter resulted in 112,000 deaths in 2013, up from 29,000 in 1990.[ten] Nevertheless, in virtually recent cases concerning the SARS-CoV‑2 pandemic, cardiac arrhythmias are commonly developed and associated with high morbidity and mortality among patients hospitalized with the COVID-19 infection, due to the infection's ability to crusade myocardial injury.[xi] Sudden cardiac death is the cause of about half of deaths due to cardiovascular disease and well-nigh xv% of all deaths globally.[12] About 80% of sudden cardiac death is the result of ventricular arrhythmias.[12] Arrhythmias may occur at whatsoever age but are more mutual among older people.[four] Arrhythmias may likewise occur in children; however, the normal range for the eye rate varies with historic period.[iii]
Nomenclature [edit]

Broad classification of arrhythmias according to region of center required to sustain the rhythm
Arrhythmia may be classified past rate (tachycardia, bradycardia), machinery (automaticity, re-entry, triggered) or duration (isolated premature beats; couplets; runs, that is 3 or more beats; non-sustained = less than 30 seconds or sustained= over xxx seconds).[ commendation needed ]
Arrhythmias are also classified by site of origin:
Atrial arrhythmia [edit]
- Sinus bradycardia
- Sinus arrhythmia
- Sinus tachycardia
- Premature atrial contractions (PACs)
- Wandering atrial pacemaker
- Atrial tachycardia
- Multifocal atrial tachycardia
- Supraventricular tachycardia (SVT)
- Atrial flutter
- Atrial fibrillation (Afib)
- AV nodal reentrant tachycardia
Junctional arrhythmia [edit]
- AV nodal reentrant tachycardia
- Junctional rhythm
- Junctional tachycardia
- Premature junctional wrinkle
Ventricular arrhythmia [edit]
- Premature ventricular contractions (PVCs), sometimes called ventricular extra beats (VEBs)
- Premature ventricular beats occurring after every normal trounce are termed ventricular bigeminy
- PVCs that occur at intervals of two normal beats to one PVC, or i normal beat to 2 PVCs, are termed "PVCs in trigeminy"[13]
- Groups of iii premature ventricular beats are called triplets and are considered a brief run of non-sustained ventricular tachycardia (NSVT); if the grouping lasts for more than xxx seconds, it is considered sustained ventricular tachycardia (VT).[14]
- Accelerated idioventricular rhythm
- Monomorphic ventricular tachycardia
- Polymorphic ventricular tachycardia
- Ventricular fibrillation
- Torsades de pointes
- Arrhythmogenic correct ventricular dysplasia
- Re-entry ventricular arrhythmia
Middle blocks [edit]
These are too known as AV blocks, considering the vast majority of them arise from pathology at the atrioventricular node. They are the most common causes of bradycardia:
- First-degree heart cake, which manifests as PR prolongation
- Second-degree centre block
- Blazon 1 Second caste heart cake, also known as Mobitz I or Wenckebach
- Type 2 2d degree heart block, also known as Mobitz Two
- 3rd-caste heart block, as well known as complete heart block.
Start, second, and third-degree blocks likewise can occur at the level of the sinoatrial junction. This is referred to equally sinoatrial block typically manifesting with various degrees and patterns of sinus bradycardia.
Sudden arrhythmic expiry syndrome [edit]
Sudden arrhythmic death syndrome (SADS), is a term used as office of sudden unexpected expiry syndrome to describe sudden death because of cardiac arrest occasioned by an arrhythmia in the presence or absenteeism of any structural heart illness on autopsy. The near common crusade of sudden death in the US is coronary artery disease specifically considering of poor oxygenation of the center muscle, that is myocardial ischemia or a eye attack[15] Approximately 180,000 to 250,000 people dice suddenly of this cause every year in the United states of america. SADS may occur from other causes. There are many inherited conditions and eye diseases that can bear upon young people which can after crusade sudden expiry without accelerate symptoms.[16]
Causes of SADS in young people include viral myocarditis, long QT syndrome, Brugada syndrome, Catecholaminergic polymorphic ventricular tachycardia, hypertrophic cardiomyopathy and arrhythmogenic right ventricular dysplasia.[17] [xviii]
Fetal arrhythmia [edit]
Arrhythmias may too occur in the fetus.[19] The normal centre rate of the fetus is between 110 and 160 beats per minute. Any rhythm beyond these limits is abnormal and classed as a fetal arrhythmia. These are mainly the outcome of premature atrial contractions, commonly give no symptoms, and take footling event. However, around one percent of these volition be the issue of significant structural damage to the eye.[19]
Signs and symptoms [edit]
The term cardiac arrhythmia covers a very big number of very different conditions.
The near common symptom of arrhythmia is an sensation of an abnormal heartbeat, called palpitations. These may exist exceptional, frequent, or continuous. Some of these arrhythmias are harmless (though distracting for patients) but some of them predispose to adverse outcomes.
Some arrhythmias practise not cause symptoms and are non associated with increased mortality. Even so, some asymptomatic arrhythmias are associated with adverse events. Examples include a higher take chances of blood clotting within the centre and a higher take chances of insufficient claret being transported to the heart because of a weak heartbeat. Other increased risks are of embolization and stroke, center failure, and sudden cardiac decease.
If an arrhythmia results in a heartbeat that is besides fast, too slow, or besides weak to supply the body's needs, this manifests as lower blood pressure and may cause lightheadedness or dizziness, or syncope (fainting).[20]
Some types of arrhythmia result in cardiac arrest, or sudden death.
Medical assessment of the abnormality using an electrocardiogram is one mode to diagnose and assess the take chances of whatsoever given arrhythmia.
Mechanism [edit]
Cardiac arrhythmia are caused by 1 of 2 major mechanism. The first of arrhythmia is a result of enhanced or abnormal impulse formation originating at the pacemaker or the His-Purkinje network. The 2nd is due to reentry conduction disturbances.[21]
Diagnostic [edit]
Cardiac arrhythmia is oft get-go detected past simple only nonspecific ways: auscultation of the heartbeat with a stethoscope, or feeling for peripheral pulses. These cannot usually diagnose specific arrhythmia merely tin requite a full general indication of the centre rate and whether it is regular or irregular. Non all the electrical impulses of the heart produce aural or palpable beats; in many cardiac arrhythmias, the premature or abnormal beats do not produce an effective pumping action and are experienced equally "skipped" beats.
The simplest specific diagnostic test for assessment of heart rhythm is the electrocardiogram (abbreviated ECG or EKG). A Holter monitor is an EKG recorded over a 24-hour flow, to detect arrhythmias that may happen briefly and unpredictably throughout the solar day.
A more advanced study of the eye'southward electric activeness tin be performed to appraise the source of the aberrant heart beats. This tin can be accomplished in an electrophysiology report, an endovascular procedure that uses a catheter to "mind" to the electrical action from within the heart, additionally if the source of the arrhythmias is institute, frequently the abnormal cells tin can exist ablated and the arrhythmia tin can exist permanently corrected. Transesophageal atrial stimulation (TAS) instead uses an electrode inserted through the esophagus to a part where the distance to the posterior wall of the left atrium is just approximately 5–half dozen mm (remaining constant in people of different age and weight).[22] Transesophageal atrial stimulation can differentiate between atrial flutter, AV nodal reentrant tachycardia and orthodromic atrioventricular reentrant tachycardia.[23] It can also evaluate the risk in people with Wolff–Parkinson–White syndrome, as well as terminate supraventricular tachycardia caused by re-entry.[23]
Differential diagnosis [edit]
Normal electrical activity [edit]
Each heartbeat originates as an electrical impulse from a small surface area of tissue in the right atrium of the middle called the sinus node or sinoatrial node (SA node). The impulse initially causes both atria to contract, then activates the atrioventricular node (AV node), which is normally the only electrical connectedness betwixt the atria and the ventricles (main pumping chambers). The impulse and so spreads through both ventricles via the bundle of His and the Purkinje fibers causing a synchronized wrinkle of the heart muscle and, thus, the pulse.
In adults, the normal resting heart charge per unit ranges from lx to 90 beats per minute. The resting middle rate in children is much faster. In athletes, however, the resting heart rate tin be every bit slow as 40 beats per minute, and be considered normal.
The term sinus arrhythmia[24] refers to a normal phenomenon of alternating balmy acceleration and slowing of the heart rate that occurs with breathing in and out respectively. It is commonly quite pronounced in children and steadily decreases with age. This can also be present during meditation breathing exercises that involve deep inhaling and breath belongings patterns.[25]
Bradycardias [edit]
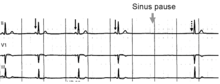
Normal sinus rhythm, with solid blackness arrows pointing to normal P waves representative of normal sinus node role, followed past a pause in sinus node activity (resulting in a transient loss of heartbeats). Note that the P wave that disrupts the pause (indicated by the dashed arrow) does not await like the previous (normal) P waves – this last P wave is arising from a different part of the atrium, representing an escape rhythm.
A tedious rhythm (less than threescore beats/min) is labelled bradycardia. This may be caused by a slowed signal from the sinus node (sinus bradycardia), by a interruption in the normal activeness of the sinus node (sinus abort), or by blocking of the electrical impulse on its way from the atria to the ventricles (AV block or middle cake). Heart block comes in varying degrees and severity. It may be caused past reversible poisoning of the AV node (with drugs that impair conduction) or by irreversible damage to the node. Bradycardias may also exist present in the normally performance middle of endurance athletes or other well-conditioned persons. Bradycardia may also occur in some types of seizures.
Tachycardias [edit]
In adults and children over 15, resting center rate faster than 100 beats per minute is labeled tachycardia. Tachycardia may result in palpitation; nonetheless, tachycardia is non necessarily an arrhythmia. Increased heart rate is a normal response to physical exercise or emotional stress. This is mediated by the sympathetic nervous organization on the sinus node and chosen sinus tachycardia. Other conditions that increase sympathetic nervous system activeness in the eye include ingested or injected substances, such every bit caffeine or amphetamines, and an overactive thyroid gland (hyperthyroidism) or anemia.
Tachycardia that is not sinus tachycardia usually results from the addition of abnormal impulses to the normal cardiac wheel. Abnormal impulses can begin by one of iii mechanisms: automaticity, re-entry, or triggered activity. A specialized form of re-entry which is both common and problematic is termed fibrillation.
Although the term "tachycardia" has been known for over 160 years, bases for the classification of arrhythmias are still existence discussed.[ citation needed ]
Center defects [edit]
Congenital middle defects are structural or electrical pathway problems in the heart that are present at nascence. Anyone can exist affected by this because overall health does not play a office in the trouble. Problems with the electrical pathway of the middle can cause very fast or even deadly arrhythmias. Wolff–Parkinson–White syndrome is due to an extra pathway in the heart that is made up of electrical musculus tissue. This tissue allows the electric impulse, which stimulates the heartbeat, to happen very rapidly. Correct ventricular outflow tract tachycardia is the most common type of ventricular tachycardia in otherwise healthy individuals. This defect is due to an electrical node in the correct ventricle only earlier the pulmonary artery. When the node is stimulated, the patient will get into ventricular tachycardia, which does non let the heart to fill with blood before beating over again. Long QT syndrome is some other complex problem in the heart and has been labeled equally an independent factor in mortality. There are multiple methods of treatment for these including cardiac ablations, medication handling, or lifestyle changes to accept less stress and exercise.
Automaticity [edit]
Automaticity refers to a cardiac muscle cell firing off an impulse on its own. All of the cells in the eye take the ability to initiate an action potential; however, but some of these cells are designed to routinely trigger heartbeats. These cells are establish in the conduction system of the heart and include the SA node, AV node, Packet of His, and Purkinje fibers. The sinoatrial node is a unmarried specialized location in the atrium that has a higher automaticity (a faster pacemaker) than the rest of the heart and, therefore, is ordinarily responsible for setting the heart charge per unit and initiating each heartbeat.
Any part of the heart that initiates an impulse without waiting for the sinoatrial node is called an ectopic focus and is, by definition, a pathological miracle. This may cause a single premature beat now and then, or, if the ectopic focus fires more than often than the sinoatrial node, it can produce a sustained aberrant rhythm. Rhythms produced by an ectopic focus in the atria, or past the atrioventricular node, are the least unsafe dysrhythmias; merely they can still produce a decrease in the centre's pumping efficiency considering the signal reaches the various parts of the heart muscle with unlike timing than usual and can be responsible for poorly coordinated wrinkle.
Conditions that increase automaticity include sympathetic nervous system stimulation and hypoxia. The resulting middle rhythm depends on where the showtime signal begins: If it is the sinoatrial node, the rhythm remains normal just rapid; if it is an ectopic focus, many types of dysrhythmia may ensue.
Re-entry [edit]
Re-entrant arrhythmias occur when an electrical impulse recurrently travels in a tight circle within the heart, rather than moving from i end of the heart to the other and then stopping.[26] [27]
Every cardiac cell can transmit impulses of excitation in every direction just will do so merely in one case within a brusk time. Normally, the action potential impulse will spread through the heart quickly enough that each cell will answer merely once. However, if in that location is some essential heterogeneity of refractory period or if conduction is abnormally slow in some areas (for example in centre damage) so the myocardial cells are unable to activate the fast sodium channel, function of the impulse will arrive tardily and potentially exist treated as a new impulse. Depending on the timing, this can produce a sustained aberrant circuit rhythm.
As a sort of re-entry, vortices of excitation in the myocardium (autowave vortices) are considered to be the principal mechanism of life-threatening cardiac arrhythmias.[28] In particular, the autowave reverberator is mutual in the sparse walls of the atria, sometimes resulting in atrial palpitate. Re-entry is also responsible for most paroxysmal supraventricular tachycardia, and dangerous ventricular tachycardia. These types of re-entry circuits are different from WPW syndromes, which utilize abnormal conduction pathways.
Although omega-iii fatty acids from fish oil can be protective against arrhythmias, they can facilitate re-entrant arrhythmias.[29]
Fibrillation [edit]
When an entire sleeping accommodation of the heart is involved in multiple micro-reentry circuits and is, therefore, quivering with chaotic electrical impulses, it is said to be in fibrillation.
Fibrillation tin can affect the atrium (atrial fibrillation) or the ventricle (ventricular fibrillation): ventricular fibrillation is imminently life-threatening.
- Atrial fibrillation affects the upper chambers of the middle, known equally the atria. Atrial fibrillation may be due to serious underlying medical weather condition and should be evaluated by a md. It is not typically a medical emergency.
- Ventricular fibrillation occurs in the ventricles (lower chambers) of the heart; it is always a medical emergency. If left untreated, ventricular fibrillation (VF, or V-fib) can lead to decease within minutes. When a eye goes into 5-fib, constructive pumping of the claret stops. V-fib is considered a form of cardiac arrest. An individual suffering from it volition not survive unless cardiopulmonary resuscitation (CPR) and defibrillation are provided immediately.
CPR can prolong the survival of the encephalon in the lack of a normal pulse, but defibrillation is the only intervention that can restore a healthy middle rhythm. Defibrillation is performed by applying an electric shock to the centre, which resets the cells, permitting a normal beat to re-constitute itself.
Triggered beats [edit]
Triggered beats occur when issues at the level of the ion channels in individual heart cells outcome in abnormal propagation of electric activity and can lead to a sustained abnormal rhythm. They are relatively rare and can result from the action of anti-arrhythmic drugs, or afterward depolarizations.
Management [edit]
The method of cardiac rhythm management depends firstly on whether the affected person is stable or unstable. Treatments may include concrete maneuvers, medications, electricity conversion, or electro- or cryo-cautery.
In the U.s., people admitted to the infirmary with cardiac arrhythmia and conduction disorders with and without complications were admitted to the intensive intendance unit of measurement more half the time in 2011.[thirty]
Physical maneuvers [edit]
Several physical acts tin increase parasympathetic nervous supply to the center, resulting in blocking of electrical conduction through the AV node. This can dull down or terminate several arrhythmias that originate in a higher place or at the AV node (see main commodity: supraventricular tachycardias). Parasympathetic nervous supply to the heart is via the vagus nervus, and these maneuvers are collectively known as vagal maneuvers.
Antiarrhythmic drugs [edit]
There are many classes of antiarrhythmic medications, with different mechanisms of action and many unlike individual drugs within these classes. Although the goal of drug therapy is to prevent arrhythmia, nearly every antiarrhythmic drug has the potential to act as a pro-arrhythmic, and so must exist advisedly selected and used nether medical supervision.
Other drugs [edit]
Several other drugs tin can be useful in cardiac arrhythmias.
Several groups of drugs wearisome conduction through the heart, without really preventing an arrhythmia. These drugs tin can be used to "charge per unit control" a fast rhythm and make it physically tolerable for the patient.
Some arrhythmias promote blood clotting within the heart and increase the gamble of embolus and stroke. Anticoagulant medications such as warfarin and heparins, and anti-platelet drugs such every bit aspirin can reduce the risk of clotting.
Electricity [edit]
Arrhythmias may also exist treated electrically, by applying a shock across the heart – either externally to the chest wall, or internally to the heart via implanted electrodes. [31]
Cardioversion is either achieved pharmacologically or via the application of a shock synchronized to the underlying heartbeat. It is used for the treatment of supraventricular tachycardias. In elective cardioversion, the recipient is commonly sedated or lightly anesthetized for the process.
Defibrillation differs in that the shock is not synchronized. Information technology is needed for the chaotic rhythm of ventricular fibrillation and is also used for pulseless ventricular tachycardia. Often, more electricity is required for defibrillation than for cardioversion. In nearly defibrillation, the recipient has lost consciousness and then there is no demand for sedation.
Defibrillation or cardioversion may be accomplished by an implantable cardioverter-defibrillator (ICD).
Electrical treatment of arrhythmias also includes cardiac pacing. Temporary pacing may be necessary for reversible causes of very slow heartbeats, or bradycardia (for example, from drug overdose or myocardial infarction). A permanent pacemaker may be placed in situations where the bradycardia is not expected to recover.
Electrical cautery [edit]
Some cardiologists further sub-specialize into electrophysiology. In specialized catheter laboratories, they use fine probes inserted through the claret vessels to map electrical action from within the center. This allows abnormal areas of conduction to be located very accurately and subsequently destroyed by rut, cold, electrical, or laser probes in a process chosen catheter ablation.
This procedure may be completely curative for some forms of arrhythmia, simply for others, the success rate remains disappointing. AV nodal reentrant tachycardia is often curable past ablating ane of the pathways in the AV node (usually the wearisome pathway). Atrial fibrillation can also be treated, by performing a pulmonary vein isolation, but the results are less reliable.
Research [edit]
Arrhythmias due to medications have been reported since the 1920s with the use of quinine.[32] In the 1960s and 1970s issues with antihistamines and antipsychotics were discovered.[32] It was not until the 1980s that the underlying issue, QTc prolongation was adamant.[32]
Run across besides [edit]
- Pre-excitation syndrome
References [edit]
- ^ a b c d "What Are the Signs and Symptoms of an Arrhythmia?". National Heart, Lung, and Blood Constitute. July i, 2011. Archived from the original on 19 Feb 2015. Retrieved 7 March 2015.
- ^ a b c d e f m "What Is Arrhythmia?". National Heart, Lung, and Blood Constitute. July 1, 2011. Archived from the original on 2 March 2015. Retrieved 7 March 2015.
- ^ a b c d e f 1000 h i "Types of Arrhythmia". National Heart, Lung, and Blood Establish. July one, 2011. Archived from the original on 7 June 2015. Retrieved 7 March 2015.
- ^ a b c d "Who Is at Hazard for an Arrhythmia?". National Heart, Lung, and Blood Constitute. July 1, 2011. Archived from the original on 3 March 2015. Retrieved 7 March 2015.
- ^ a b "How Are Arrhythmias Diagnosed?". National Heart, Lung, and Claret Plant. July 1, 2011. Archived from the original on 18 February 2015. Retrieved 7 March 2015.
- ^ a b c d e f g "How Are Arrhythmias Treated?". National Center, Lung, and Blood Institute. July 1, 2011. Archived from the original on 17 Feb 2015. Retrieved 7 March 2015.
- ^ Martin CA, Matthews GD, Huang CL (April 2012). "Sudden cardiac expiry and inherited channelopathy: the basic electrophysiology of the myocyte and myocardium in ion channel illness". Center. 98 (vii): 536–543. doi:10.1136/heartjnl-2011-300953. PMC3308472. PMID 22422742.
- ^ Vogler J, Breithardt G, Eckardt L (July 2012). "Bradyarrhythmias and conduction blocks". Revista Espanola de Cardiologia. 65 (7): 656–667. doi:ten.1016/j.rec.2012.01.027. PMID 22627074.
- ^ Zoni-Berisso 1000, Lercari F, Carazza T, Domenicucci S (2014). "Epidemiology of atrial fibrillation: European perspective". Clinical Epidemiology. 6: 213–220. doi:x.2147/CLEP.S47385. PMC4064952. PMID 24966695.
- ^ GBD 2013 Mortality Causes of Death Collaborators (January 2015). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Brunt of Disease Study 2013". Lancet. 385 (9963): 117–171. doi:10.1016/S0140-6736(14)61682-2. PMC4340604. PMID 25530442.
- ^ Kuck KH (June 2020). "Arrhythmias and sudden cardiac death in the COVID-19 pandemic". Herz. 45 (4): 325–326. doi:10.1007/s00059-020-04924-0. PMC7181098. PMID 32333026.
- ^ a b Mehra R (2007). "Global public health trouble of sudden cardiac expiry". Journal of Electrocardiology. forty (6 Suppl): S118–S122. doi:ten.1016/j.jelectrocard.2007.06.023. PMID 17993308.
- ^ "Trigeminy PVC: Definition, Causes, Treatment". 26 February 2018.
- ^ Wagner GS (2001). Marriott's Practical Electrocardiography (tenth ed.). Philadelphia, PA: Williams & Wilkins. ISBN0683307460. [ page needed ]
- ^ Zipes DP, Wellens HJ (November 1998). "Sudden cardiac death". Apportionment. 98 (21): 2334–2351. doi:10.1161/01.CIR.98.21.2334. PMID 9826323.
- ^ Deo R, Albert CM (January 2012). "Epidemiology and genetics of sudden cardiac death". Circulation. 125 (4): 620–637. doi:10.1161/circulationaha.111.023838. PMC3399522. PMID 22294707.
- ^ Chugh SS, Reinier K, Teodorescu C, Evanado A, Kehr E, Al Samara M, et al. (2008). "Epidemiology of sudden cardiac death: clinical and research implications". Progress in Cardiovascular Diseases. 51 (3): 213–228. doi:ten.1016/j.pcad.2008.06.003. PMC2621010. PMID 19026856.
- ^ Winkel BG, Holst AG, Theilade J, Kristensen IB, Thomsen JL, Ottesen GL, et al. (April 2011). "Nationwide report of sudden cardiac death in persons anile 1-35 years". European Centre Journal. 32 (8): 983–990. doi:x.1093/eurheartj/ehq428. PMID 21131293.
- ^ a b Batra As, Balaji S (2019). "Fetal arrhythmias: Diagnosis and management". Indian Pacing and Electrophysiology Periodical. 19 (3): 104–109. doi:10.1016/j.ipej.2019.02.007. PMC6531664. PMID 30817991.
- ^ "Passing Out (Syncope) Caused by Arrhythmias". Retrieved 13 April 2020.
- ^ Antzelevitch C, Burashnikov A (March 2011). "Overview of Basic Mechanisms of Cardiac Arrhythmia". Cardiac Electrophysiology Clinics. 3 (1): 23–45. doi:10.1016/j.ccep.2010.ten.012. PMC3164530. PMID 21892379.
- ^ Anier A, Kaik J, Meigas Yard (2008). "Device and methods for performing transesophageal stimulation at reduced pacing current threshold". Estonian Journal of Technology. 57 (2): 154. doi:10.3176/eng.2008.2.05. S2CID 42055085.
- ^ a b Pehrson SM, Blomström-Lundqvist C, Ljungström E, Blomström P (October 1994). "Clinical value of transesophageal atrial stimulation and recording in patients with arrhythmia-related symptoms or documented supraventricular tachycardia--correlation to clinical history and invasive studies". Clinical Cardiology. 17 (10): 528–534. doi:x.1002/clc.4960171004. PMID 8001299. S2CID 7097362.
- ^ Yasuma F, Hayano J (February 2004). "Respiratory sinus arrhythmia: why does the heartbeat synchronize with respiratory rhythm?". Chest. 125 (2): 683–690. doi:10.1378/chest.125.2.683. PMID 14769752.
- ^ Peressutti C, Martín-González JM, M García-Manso J, Mesa D (November 2010). "Heart rate dynamics in unlike levels of Zen meditation". International Journal of Cardiology. 145 (1): 142–146. doi:x.1016/j.ijcard.2009.06.058. PMID 19631997.
- ^ Wiener N, Rosenblueth A (July 1946). "The mathematical conception of the problem of conduction of impulses in a network of connected excitable elements, specifically in cardiac muscle". Archivos del Instituto de Cardiologia de Mexico. xvi (3): 205–265. PMID 20245817.
- ^ Allessie MA, Bonke FI, Schopman FJ (August 1976). "Circus movement in rabbit atrial muscle every bit a machinery of tachycardia. II. The part of nonuniform recovery of excitability in the occurrence of unidirectional block, as studied with multiple microelectrodes". Apportionment Research. 39 (2): 168–177. doi:10.1161/01.RES.39.2.168. PMID 939001.
- ^ Mandel WJ, ed. (1995). Cardiac Arrhythmias: Their Mechanisms, Diagnosis, and Management (3 ed.). Lippincott Williams & Wilkins. ISBN978-0-397-51185-three. [ page needed ]
- ^ Den Ruijter HM, Berecki G, Opthof T, Verkerk AO, Zock PL, Coronel R (January 2007). "Pro- and antiarrhythmic properties of a diet rich in fish oil". Cardiovascular Research. 73 (2): 316–325. doi:10.1016/j.cardiores.2006.06.014. PMID 16859661.
- ^ Barrett ML, Smith MW, Elizhauser A, Honigman LS, Pines JM (December 2014). "Utilization of Intensive Intendance Services, 2011". HCUP Statistical Brief #185. Rockville, MD: Agency for Healthcare Inquiry and Quality. Archived from the original on 2015-04-02.
- ^ "AED Heir-apparent's Guide | AED Prices & Comparing". AED Brands . Retrieved 2021-08-xiii .
- ^ a b c Heist EK, Ruskin JN (Oct 2010). "Drug-induced arrhythmia". Apportionment. 122 (14): 1426–1435. doi:x.1161/circulationaha.109.894725. PMID 20921449.
External links [edit]
- Arrhythmia at Curlie
Source: https://en.wikipedia.org/wiki/Arrhythmia
0 Response to "what refers to erratic, irregular contractions of the cardiac muscle"
Post a Comment